Different Types Of Covid-19 Tests
With an extensive array of testing options at various health care facilities, most people battle with picking the appropriate test option. Others even wonder if they all work the same way.
The truth is there is no single testing strategy with the capacity to meet each need and at the same time solve every COVID-based challenge. However, the right testing approach should be based on the testing objective, such as determining whether an individual might have been previously infected in the past or determine whether someone has an active COVID infection.
The following are some of the different types of COVID-19 test

PCR, RNA, Or Molecular Test
Molecular testing is believed to be the most accurate for detecting active infections. You may be advised to take an RNA test if your doctor or you suspect you have the infection. This test follows the typical testing approach, but some recent RNA tests involve the swabbing of saliva. The improvement time for molecular testing can differ from minutes to days or even longer. It’s all hinged on whether the sample is analyzed outside the lab or onsite.
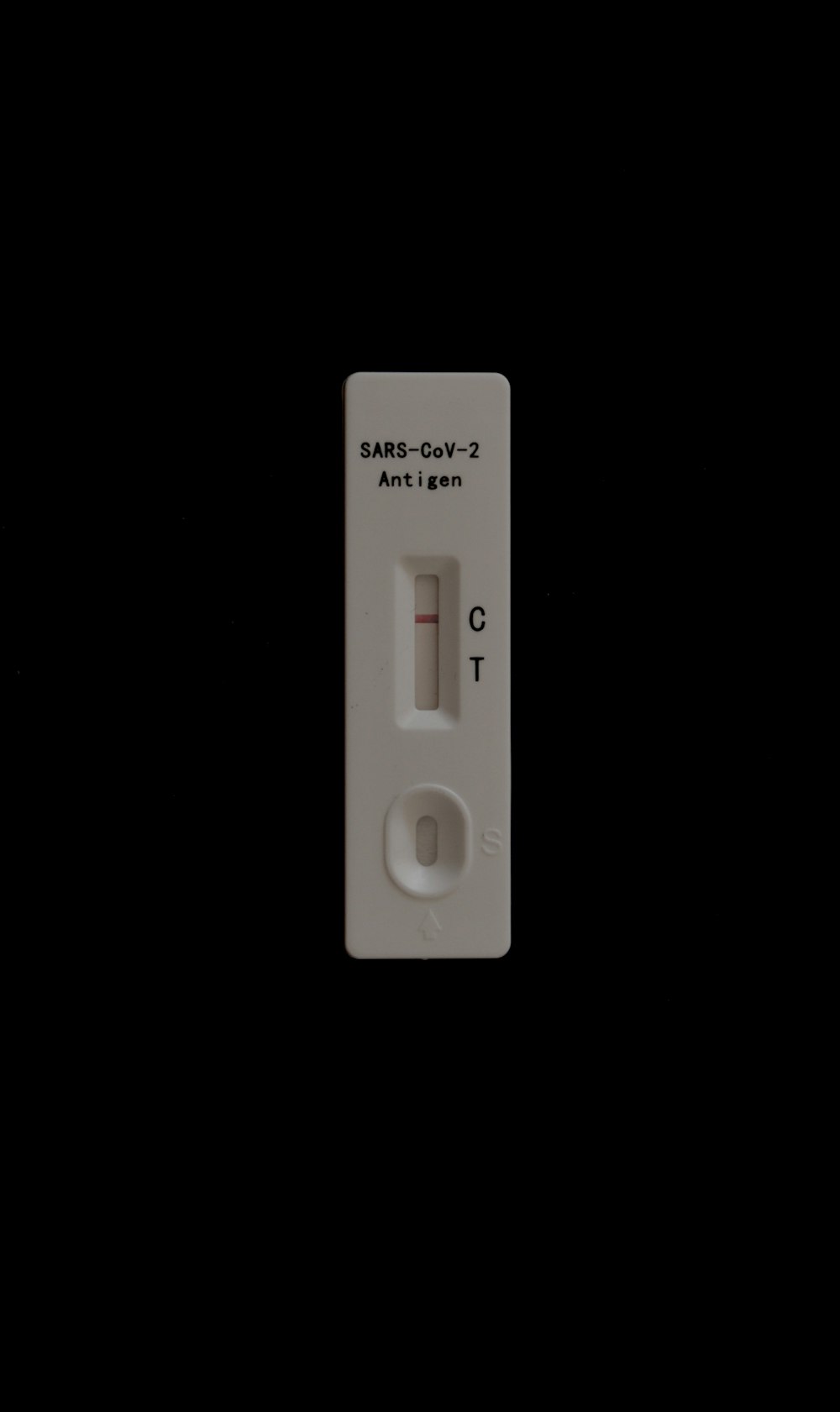
Rapid Or Antigen Test
Antigen test is commonly referred to ‘rapid test’ based on the improvement time. These tests are faster and cheaper to produce than molecular test. An article in the journal nature suggests that the quick turnaround of rapid tests explains why it is used to test large numbers of people. This test works almost like the RNA test. The back of your throat or nose would be swabbed by a health practitioner to collect a sample for testing. However, you’ll get your result within minutes or hours instead of agonizingly waiting for days to see the results. Although, if you test positive, the result is probably accurate, the flip side of the antigen test is that it’s more likely to miss active infections.
Blood , Antibody Or Serology Test
The aim of this testing approach is to determine if you have been previously infected, so it detects antibodies. These antibodies are proteins that your immune system generates to combat a virus. However, antibody tests cannot test for active antigen.
According to Mayor Clinic, serology testing is not endorsed until 14 days after the patient starts to experience COVID-19 symptoms. The question then is, if a person has antibodies to SAR-CoV-2, does that suggest that that person is immune against future COVID infections? That’s hard to say since researchers are not certain about this. However, recent investigations have insinuated that past attacks may offer some protection against the pandemic.
Tips For Building A Robust COVID-19 Testing Strategy
Testing is a significant factor for the control and prevention of the virus.
Availability Of Resources And Tools
According to the WHO, it is recommended that every country have a national testing strategy with available resources and tools to preserve the highest level of public health impact. Substitute measures and public health interventions can be implemented if testing capacity is low.
Well-Defined Objectives And Prioritization Of Testing Strategy
Countries should also have well-defined goals that can be modified based on the shifts in epidemiological conditions. Although the testing of symptomatic patients should be ranked above the tests of asymptomatic individuals. Nevertheless, testing of asymptomatic patients can be enlightening in cases like testing of medical care and longstanding care facility workers that are frequently exposed or follow up of contacts of confirmed or probable cases.
Country-Based Context
There should be an extensive application of diagnostics in prevalent asymptomatic population screening as well as self-testing for SARS-CoV-2. Demographic factors such as the existence of vulnerable groups (e.g. migrant, refugee, or displaced populations) or population density, should be considered since it has the capacity to influence the availability and type of testing approach.
Country-based context is also significant because it can influence decision-making in countries with protracted or complex emergencies, low- and middle-income nations, or small island developing states.
Finally, it is important that all SARS-CoV-2 testing is connected to public health activities to guarantee proper medical care and assistance and to execute contact tracing to dismantle chains of transmission. The pandemic has emphasized the significance of a resilient, well-resourced, and dependable laboratory network. It also offers an opening to implement resources and reinforce country capability for detection of SARS-CoV-2 and other epidemic-prone viruses. Hence, preparedness and surveillance for COVID-19 response should be always preserved.

References
Duncan, A. (2020, October 7). The 3 types of COVID-19 tests, and what each one tells you. Health.com. Health
Nimer, S. D., Chapman, J., Reidy, L., Alencar, A., Wu, Y., Williams, S., Pagan, L., Gjolaj, L., MacIntyre, J., Triana, M., Vance, B., Andrews, D., Fan, Y., Zhou, Y., Martinez, O., Garcia-Buitrago, M., Cray, C., Tekin, M., McCauley, J. L., … Jorda, M. (2020). A how-to guide to building a robust SARS-Cov-2 testing program at a university-based health system. Academic Pathology, 7. Nimer
WHO. (2021, June 20). Recommendations for national SARS-CoV-2 testing strategies and diagnostic capacities. World Health Organization (WHO). WHO

